Intermittent stagnation and ketogenic also have the chance to reduce dementia risks! The doctor reveals that "1 factor" is the key

Text/Richard Restark
Many researchers pointed out that intermittent cessation has some benefits for patients with Alzheimer's disease (more discussed in detail later), and we will focus on the changes in the brain during the cessation process.
After twelve to thirty-six hours of eating, the body will enter the physiological state of "ketopathy", with low blood sugar and excessive consumption of liver sugar (also known as glycogen). Hepatitis is a glucose storage body produced by the liver. During the course of the cessation, the liver sugar will be decomposed from glucose continuously, and after a few hours, the liver sugar will be completely consumed. In response to this situation, cells in other parts of the body will release fat. Fat flows back to the liver with the blood, where it is converted into ketones, another source of energy for the body when glucose is not available. This "representation conversion" occurs twelve hours after the meal, and the ketone body will replace glucose.
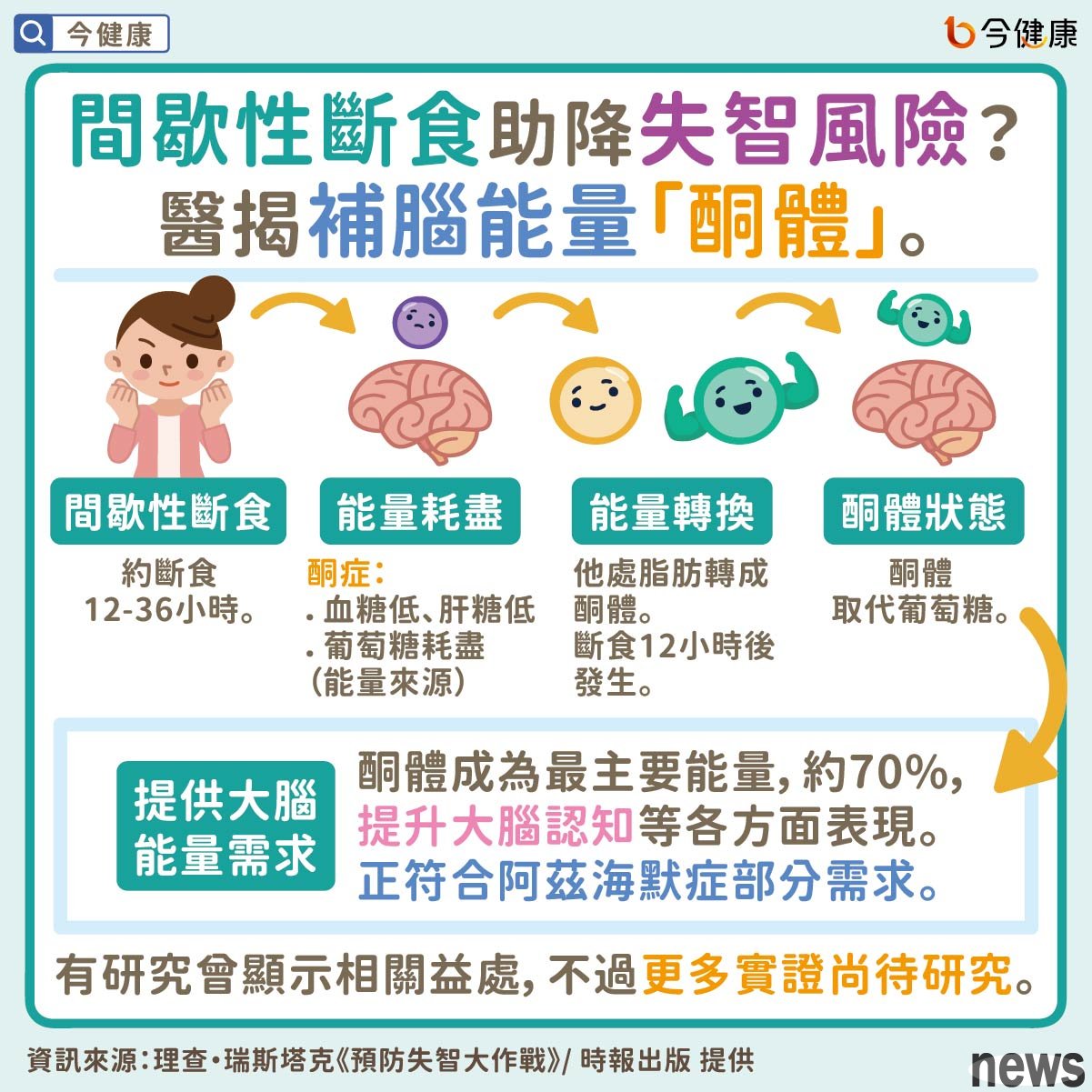
Although the liver is the main part of ketone production, astrocytes in the brain can also produce ketones. After a few hours of starting a meal, ketones become the main source of energy for the brain, providing 70% of its energy needs. Ketones are an efficient source of energy in muscles and can also enhance the bioenergy and cognitive performance of brain cells. This kind of keratinization conversion can be produced based on the principles of the ketogenic diet: high fat, appropriate protein, and low carbohydrates.
In animal experiments, mice that received a five-day ketogenic diet performed better in space learning and memory. People with Alzheimer's disease also need to increase the bioenergy of neuronal cells, stabilize glucose induced by signal transmission.

The efficacy of ketogenic diet is similar to that of off-dining, and the effects it brings are similar, and can also produce ketones. But what impact will this kind of credit conversion have on the brain?
Many people say that entering the "keto state" can make people feel hyperactive, happy and open-minded. Some people may feel suddenly awake. Most importantly, eating out can enhance thinking, learning, memory and alertness because this process stimulates a protein in the brain cells: "brain-derived neuron nutrition factor." This chemical substance has the greatest impact on the macaque, helping the production of middle neurons, thus improving memory. Diet will also cause "autophagy": destroying or removing nerve cells that are damaged and abnormally functional.
From a direct perspective, ketogenic diet should be helpful in treating Alzheimer's disease, because the patient's brain cannot absorb glucose, but can still use ketones normally. However, so far, there has not been enough research to prove the benefits of ketogenic diets. But one study showed that fifteen patients with mild to moderate Alzheimer's disease said their cognitive ability improved after a 12-week ketogenic diet.
However, many people's physical condition is not suitable for quitting, so you must consult the doctor's opinion before practicing. Overall, eating out may become a way to reduce the risk of dementia, so see if more studies can prove the positive effects of ketogenic diets.

《